Testing For Coronavirus: 2 Things You Absolutely Need To Know About How Its Done
As the armies of novel coronavirus continue their relentless march across the world, conquering city after city, and country after country, one of the most vital assets in our hands to try and slow down their spread is to detect the virus in people and on objects. This is what the COVID tests are all about. All the statistics regarding the daily new cases, active cases and recovered cases, are based on the outcomes of these tests, which is why countries the world over are trying hard to conduct as many tests as possible on a daily basis.
But how reliable are these tests really? What are their limits? And what inferences can we derive from them? These are the questions I will address in this post.
There Are Two Ways To Detect Coronavirus
There are two different ways that the presence of coronavirus in a person or on an object can be detected, and they use two different categories of molecules to detect the virus. The first is PCR (Polymerase Chain Reaction). This test detects coronavirus RNA, which is the genetic material that carries the genes of coronavirus. As its name suggests, RNA is closely related to its more well known cousin, DNA. You can read about how DNA and RNA store genetic information in this post by me, and how DNA and RNA differ from each other in this post by me.
A PCR based test is extremely sensitive. So it can detect even tiny traces of coronavirus RNA in a sample. It does this through a chain reaction, in which one copy of coronavirus RNA generates multiple copies of itself, each of which in turn generate even more copies and so on, until the amount of copies are large enough to be experimentally detected. This is a bit like a tiny little spark causing a massive explosion in a factory. Those familiar with mathematics will know it as exponential increase, or geometric progression.
The other kind of test used to detect coronavirus is an antibody based test, also called a serological test. When coronavirus, or any other foreign microbe for that matter, enters our body, our immune system generates antibody molecules that recognize specific molecules on the microbe and bind to them. This way, the immune system detects the microbe and eliminates it. An antibody test detects the presence of antibodies specific to coronavirus in a person’s blood. If the presence of these anti-coronavirus antibodies is detected, it logically means that the patient was either infected by coronavirus in the past, or is currently infected.
Using PCR To Detect Coronavirus On An Object Doesn’t Confirm The Presence Of Intact Virus On It
There have been two main studies so far, to see if coronavirus remains viable on surfaces like metal, plastic and cardboard for a long period of time. One of these was published by The New England Journal of Medicine and the other by The Lancet. These studies involved taking swabs of surfaces and applying them to mammalian cells, like the Vero E6 cells, that are susceptible to infection. Infection in these cells after applying the swab would prove beyond doubt that the surfaces have intact coronavirus.
Some other studies like this one, however, involved taking swabs of people as well as the surfaces and checking them for the presence of coronavirus RNA using PCR. However, there is a problem with this approach. RNA, just like DNA, is a highly stable molecule that doesn’t degrade easily. The virus itself, however, might be far more fragile than its RNA. This means that the RNA of the virus can easily outlast the virus itself.
So, the presence of viral RNA or DNA on an object shows the the virus was present on the surface at some time. But it doesn’t necessarily mean that the virus might still be intact. The study mentioned above actually mentions that mare presence of viral RNA on an object does not confirm the presence of viable virus on it, and more studies need to be done. But despite this caveat, the media and the public give undue importance to the fact that coronavirus RNA was found on surfaces for 17 days, like mentioned in this post.
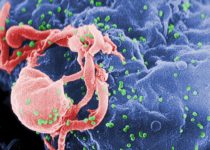
In fact, other viruses like HIV and influenza don’t survive for more than 3 to 5 minutes outside human body, as their structure is very fragile. And these viruses are similar in structure to coronavirus. You can read all about the molecular structure of coronavirus in this post of mine.

An example of how far molecules like DNA and RNA can outlive the organism they belonged to, can be seen in the fact that mammoth fossils that are tens of thousands of years old have been found to contain fragments of intact mammoth DNA. In fact, researchers are trying to insert these mammoth DNA fragments into elephant DNA to produce mammoth-elephant hybrids. Even the basis of the movie Jurassic Park is that dinosaur DNA preserved in mosquitoes who sucked their blood, who in turn are preserved in amber, can theoretically be used to resurrect the ancient reptiles. The studies that only use PCR to detect the presence of coronavirus on objects, therefore, should be taken with a grain of salt.
Then what situation is the PCR based detection of coronavirus truly useful in? Its when you use it to test if a person is COVID positive. Because inside a patient’s body, the virus stays intact until the person recovers. The person tests psitive if the viral RNA is detected in his blood through PCR, and is said to have completely recovered once he tests negative, or in other words, when PCR test doesn’t find any viral RNA in his blood.
There are also instances in which a person who has stopped showing COVID symptoms for a long time, and has completed the quarantine period, is considered recovered even if he continues to test positive. This is again because being a highly stable molecule, a tiny bit of viral RNA might outlast the virus itself in the patient’s body. And being an extremely sensitive test, PCR might detect this tiny bit of residual viral RNA, which should not be interpreted as presence of intact virus in the body.
Antibody Tests Might Not Be As Accurate As We Want
Antibody tests have one major advantage over PCR tests- they can be much faster, giving results in a matter of minutes. All you have to do is apply a patient’s blood on a ready made kit that detects antibodies against the virus, and the results are out. Antibody tests are not just used to detect infections and immunity to them, but for many other purposes. One of the most common antibody tests is the one carried out for identification of blood groups based on agglutination. Moreover, antibodies are not just used in these tests, but in biological research in general.
The problem, however, is that the antibodies aren’t always as specific as one would like them to be. Companies commercially produce antibodies specific to various molecules and mention their specificity in their catalog. But its a standard practice in most labs, to still test the specificity of these antibodies, as they are often found to bind not only to their target molecule, but also to other molecules. In fact in experiments involving antibodies, like western blot, the problem of antibody non specifically binding to other molecules is so pronounced that we need to use either bovine serum albumin, or skimmed milk, to mask all the regions where the antibody might non specifically bind.
Despite this, the tendency of antibodies to non specifically bind has been a real nuisance in research. As the video below says, in 2011, an analysis was published in the journal Nature Structural and Molecular Biology, in which 246 different commercially available antibodies, that were claimed to specifically bind only one unique molecule, were tested for their specificity. The results showed that contrary to the claims, a quarter of these antibodies bound to more than one molecule, and four of them did not even bind to the molecule they were claimed to bind.
This non specific binding creates actual hardships. For example, researchers at Mount Sinai Hospital in Toronto, spent two years and half a million dollars trying to detect a protein believed to be connected to pancreatic cancer, using an antibody claimed to be specific to that protein. Eventually however, it was fund that the antibody actually binds to the wrong protein molecule. As the video below shows, this is just a part of a larger problem of reproducible crisis in research, which you can read more about in this post of mine. The companies commercially producing antibodies are starting to improve their quality control. But the problem persists.
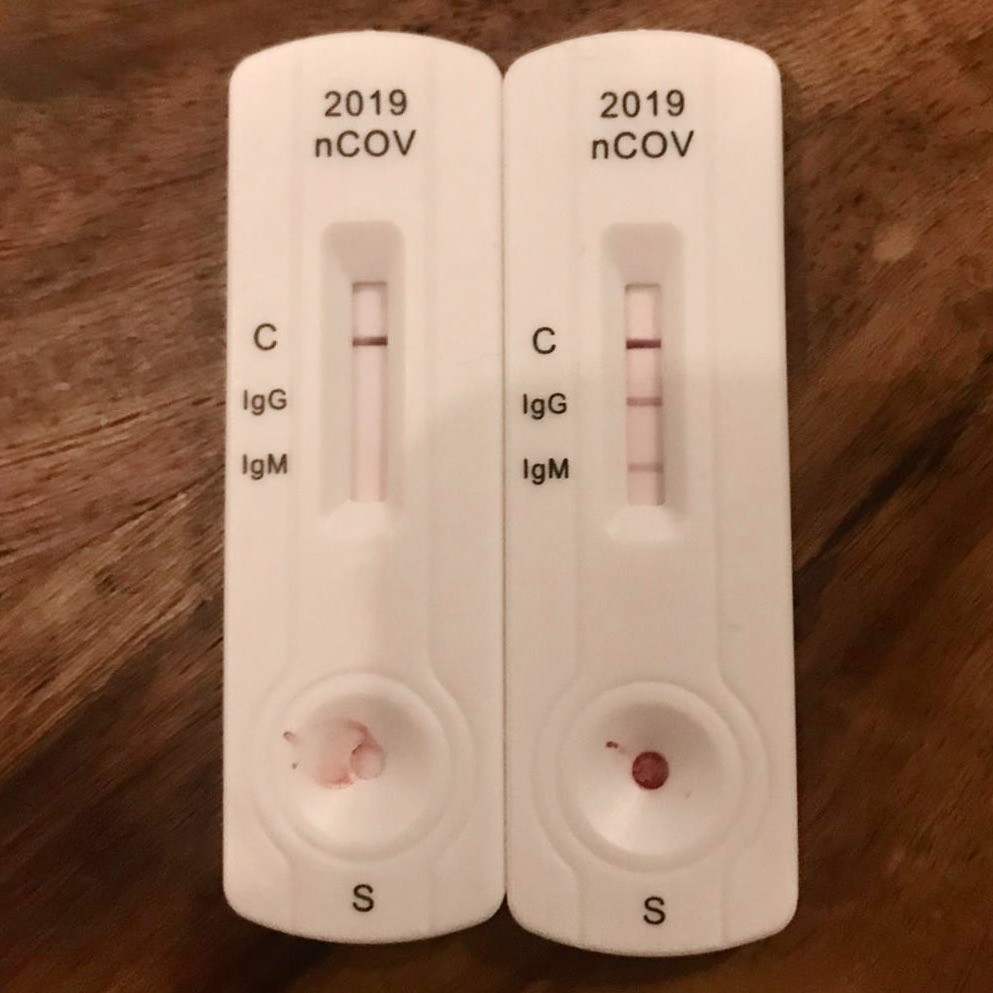
So what are the implications of this non specificity of antibodies for the large scale antibody testing to detect coronavirus? A large scale survey done in Delhi using rapid antibody tests suggests about 25% of the total population of Delhi now carries antibodies against coronavirus. This would suggest that 25% of the population has been infected by the virus. These tests detect two different kinds of antibodies against coronavirus, namely IgM and IgG. The amount of IgM antibodies suddenly increases right after infection by a microbe, and goes down after a while. But the amount of IgG antibodies, increases slowly after the infection and stays high for a long period, even after the person has recovered.
So, high IgM in a person’s blood would indicate that he is currently infected by the virus, while no IgM and high amount of IgG would indicate that he was infected by the virus in the past, but has now recovered. But if commercially produced antibodies can non specifically bind to molecules they are not supposed to bind, its possible that the antibodies in a person’s blood, might have been produced against a different virus in the past, and is only non specifically binding to the molecules of coronavirus in the antibody tests.
This doesn’t in any way mean that the findings of these large scale antibody tests should be ignored. But they should certainly be taken with a grain of salt, and more studies should be done to gauge the extent of non specific binding of antibodies to coronavirus molecules.
This Does NOT Mean You Should Write Off Test Results As False
These facts certainly have a sobering effect on our enthusiasm in using PCR and antibody tests to detect coronavirus. But this doesn’t in any way mean that we can discount the findings of these tests as false and ignore them. What most people fail to realize is that science and research is far murkier than we would like it to be, for better or for worse. In other words, it’s complicated. It’s just how science progresses.
The way to go is to use these findings as justification to study to what extent they affect our understanding of how coronavirus spreads and how to deal with it, and refine our methods to obtain a more accurate picture of the virus and the pandemic it has caused.